Patellofemoral dislocation accounts for fewer than 3% of knee injuries seen by most orthopedic surgeons. Evaluating patellofemoral dislocation and determining whether surgical or non-surgical management is the best treatment for a particular patient is difficult due to anatomical complexity and challenges in determining the cause of the instability.
A Nuanced Plan
“These patients require a nuanced evaluation and treatment plan that’s developed by knee specialists who see a high volume of patellofemoral dislocation,” says Rodney Benner, MD, an orthopedic surgeon at Shelbourne Knee Center. Dr. Benner and K. Donald Shelbourne, MD, also an orthopedic surgeon at Shelbourne Knee Center, have performed surgery on more than 700 patients with patellofemoral dislocation.
In patients with instability due to an anatomic predisposition, dislocation often occurs in both knees and can be caused by mild trauma, daily activities or major trauma. Other patients experience patellofemoral dislocation after a traumatic injury in an otherwise normal knee. The best treatment depends upon the cause of the instability.
Research-Based Algorithm
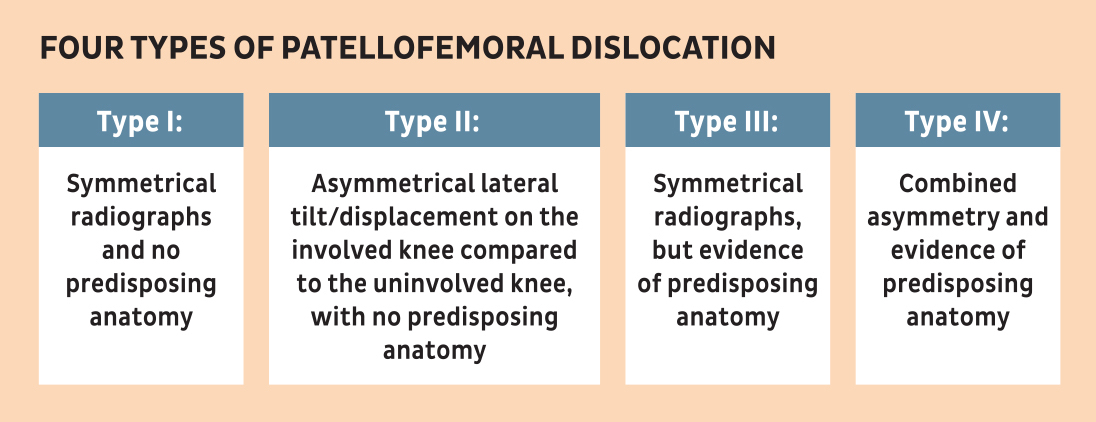
Shelbourne Knee Center’s algorithm for managing patellofemoral dislocation starts with determining whether there are any predisposing factors associated with the patellar dislocation and physical and radiographic evaluation of both knees. Using a plain radiograph-based classification system developed at Shelbourne Knee Center,1 Dr. Benner and Dr. Shelbourne classify the patellofemoral dislocation according to symmetry between the knees and evidence of predisposing anatomy. The radiographs are the bilateral Merchants’ view and 60-degree lateral view of both knees.
Surgical Versus Non-Surgical Treatment
The classification and the impact of instability on the patient’s life help Dr. Benner and Dr. Shelbourne determine the best treatment. For patients with first-time dislocations, Shelbourne Knee Center’s research-based rehabilitation program is usually the initial treatment. “Soft tissues will heal on their own,” says Dr. Benner. “We help the patient reduce swelling and then regain range of motion through our rehabilitation program. Once the patient can straighten the knee, he/she transitions to low-impact exercise and strengthening to return strength to normal.”
Surgery is usually indicated to prevent further dislocation for patients with:
- Predisposing anatomical factors for patellar dislocation
- First-time patellofemoral dislocation with asymmetry and a malaligned patella
- Multiple patellofemoral dislocations.
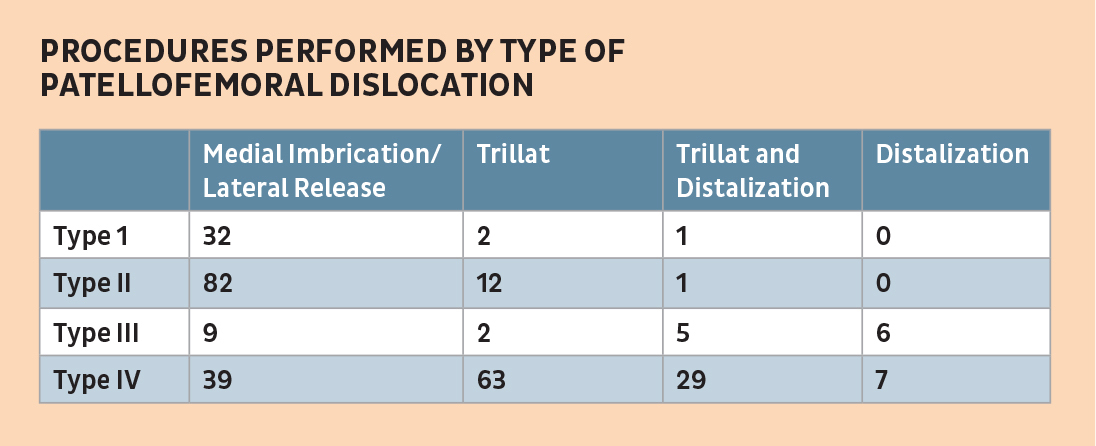
If surgery is indicated, the patient’s classification is used to determine the best procedure. Surgical patients complete preoperative physical therapy to prepare for surgery and postoperative physical therapy to control swelling, regain range of motion and regain leg strength and function.
Patellofemoral Dislocation Classification System
In developing the patellofemoral dislocation classification system, Shelbourne Knee Center classified 290 patients who were treated operatively for patellofemoral instability/dislocation between February 2003 and May 2019 based on their pre-operative radiographs.1 Researchers evaluated the Merchants’ view radiograph for symmetry between the knees for placement of the patella in the trochlear groove. They considered evidence of linear displacement, lateral tilt, and patella-alta in determining predisposing anatomy.
Researchers divided patients into one of four classifications.
Postoperatively, researchers compared preoperative and postoperative radiographs to determine if surgery successfully corrected for the identified asymmetry and/or predisposing anatomy. They measured interrater reliability between the operating surgeon and a research associate with a blinded sample group of 51 patients and intrarater reliability with a blinded sample group of 50 patients treated for patellofemoral instability who were age/sex matched to patients without patellofemoral instability.
Results
Intrarater reliability was 96% (n=100) and interrater reliability was 98% (n=51). Patients were classified as:
- Type I: 12% (n=35)
- Type II: 33% (n=95)
- Type III: 8% (n=22)
- Type IV: 48% (n=138).
Comparing preoperative and postoperative radiographs, 99% of patients’ surgery corrected for the intended asymmetry and/or predisposing anatomy.
Researchers concluded that this novel classification system may help facilitate communication between providers, guide further research into surgical options and assist surgeons in treatment decision-making.
References
- Benner RW, Shelbourne KD, Bailey JM. A Novel Radiograph System for Classifying Patellofemoral Instability Based on Symmetry and Predisposing Anatomy. Unpublished abstract. Shelbourne Knee Center, 2020.
- Shelbourne KD, Urch SE. Results of Medial Retinacular Imbrication in Patients with Unilateral Patellar Dislocation. J Knee Surg. 2012;25:391–396.