Osteoarthritis is the degeneration of the joint—a disease process causing the joint surface to wear away. The symptoms can include all or some of the following: pain, stiffness, swelling, warmth, loss of motion, decreased activity, tenderness and crepitus (grinding). Causes of osteoarthritis include age, sex, obesity, genetic disposition, bone deformities, certain metabolic diseases, previous injury or surgery and repetitive high-impact activities. The knee becomes painful and limiting over time, not suddenly, because of a cycle that patients aren’t generally aware of. This cycle looks something like this:
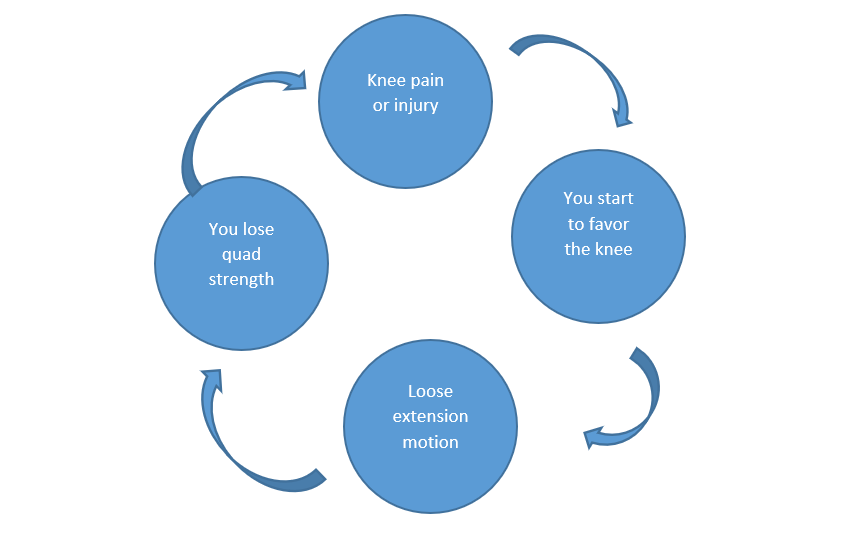
The pain that starts from either an injury or a meniscus tear will cause a person to decrease their activity and not use the leg normally, hoping the pain will resolve on its own. However, by not using the knee normally, favoring and decreasing activity leads to increased stiffness, which then leads to quad weakness. This will cause more pain in the joint and not help the knee feel better. So, until the cycle is broken with the correct exercises and progression of exercises, the knee continues to get stiffer and weaker. This is when individuals end up in doctors’ offices seeking relief from the pain and a return to their previous quality of life.
Typical Treatment
In a typical doctor’s office visit, emergency room, primary care or orthopedic practice, there will be X-rays to make sure nothing is broken and medications. Often, patients will be advised to decrease or modify activities, put a pillow under the knee to improve nighttime comfort, and then return if the pain does not get better. All of these recommendations will not make the knee better and get one back to normal activities. In fact, this may provide some very short-term relief, but the reality is this will often make the knee continue to feel worse. In some cases, the physician may offer an arthroscopy to “clean up” the arthritis. It is important to understand that you cannot “clean up” arthritis. Other treatment options may include braces, medications, injections, activity modifications, shoe inserts, supplements, heat, cold, weight loss, and ultimately surgery. However, none of these methods can improve range of motion or improve strength.
Our Philosophy
At Shelbourne Knee Center, we follow our patients long-term through research so that we can make sure individuals are doing well and are able to return to the activities they want. By doing this over the past 30+ years, we have been able to improve how we treat patients and make sure we are maintaining the highest standards of care.
Our philosophy is to teach patients how to get their range of motion back to normal, particularly extension (getting the knee straight) so that they can start increasing strength in order to return to normal activities they enjoy. Our research shows that improvements in extension and flexion (bending) allow for a more successful return of quad strength. Instead of having patients come to physical therapy weekly for multiple weeks, we see them a handful of times over a longer duration to teach them how to progress and manage their arthritic knee long-term in hopes of avoiding a knee replacement.
If a patient improves range of motion and strength, but the pain and function of the knee is not where he or she wants it to be, then a discussion can be had to move forward with a knee replacement. But this is always the last option when all the nonoperative treatments have been tried and are no longer effective. The knees should be mirror images of each other, and our goal is to achieve that symmetry. We only treat knees and our experience has taught us that individuals can improve the pain and function of the knee by restoring range of motion and strength.

