
Unfortunately, ACL tears cannot heal on their own. A normal ACL provides stability to the knee joint during activities such as cutting, pivoting, and jumping. A patient to wishes to return to their previous level of activity in sports that require these types of movements should have the torn ACL surgically reconstructed.
For patients that tear their ACL but do not plan on performing these types of activities, reconstruction surgery may not be needed. You do not need an intact ACL in order to perform daily activities or straight-forward exercises, like walking and running. We will review these options with you during your appointment.
For patients that choose to have the ACL reconstructed, the treatment would consist of 3 phases:
- Pre-op physical therapy (rehab) to prepare you for surgery and help you recover faster afterwards.
- Surgery that uses the strongest graft available to reconstruct your ACL.
- Post-op physical therapy (rehab) that prevents swelling and helps you recover quickly.
Learn More About Our Treatments for ACL Injuries
ACL RECONSTRUCTION
Anterior cruciate ligament (ACL) reconstruction creates a new ligament inside your knee to replace the torn ACL and restore stability to the knee joint.
Physical Therapy Before ACL Surgery
PRE-OP Physical Therapy
The purpose of physical therapy before surgery is to get you prepared both physically and mentally.
Before scheduling surgery, the following conditions must be met:
- Full range of motion.
- Little or no swelling.
- Normal walking.
- Appropriate strength.
Returning your injured knee to a normal state (except for the ACL tear) will speed up recovery time and allow goals after surgery to be more easily achieved. How long it takes to get your knee to become ready for surgery varies from person to person, but is generally 2-4 weeks.
Before surgery, you and your caregiver (the person that will take care of you for the first 7 days after surgery) will return for a surgery talk and test visit. This visit consists of performing a series of tests that measure your strength and stability on both legs to ensure you return to your previous level of function after surgery. We will also provide education on the surgery itself, time spent in the hospital, physical therapy exercises, and post-op goals and expectations.
Graft Choice
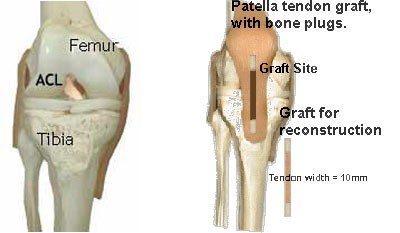
The tendon used to replace your torn ACL is called a graft. There are several types of grafts available to reconstruct the ACL, such as the patellar tendon, hamstring tendons, or cadaver (allograft). We choose the patellar tendon to reconstruct the torn ACL over other grafts because it is the strongest graft with the highest success rate.
The graft can be taken from either knee. However, after years of experience, we have found that taking the graft from the opposite (contralateral) knee allows for a faster, more predictable recovery. You can choose which knee to use for the graft. Sometimes, there are medical reasons for us to recommend which knee should be used for the graft.
Arthroscopy
ACL reconstruction surgery begins with an arthroscopy (scope). This procedure is used to examine the knee joint and look for meniscal and/or bone surface damage, which occurs at the time of the ACL tear. These injuries are treated at this time.

Remove ACL and Clean Notch
Following the scope, ACL reconstruction begins with an incision in the front of the knee. After exposing the knee joint, the damaged ACL is removed and the area where the ACL normally resides (intercondylar notch) is cleaned to make room for the new ACL graft.
Tunnels for The Graft
Tunnels* are drilled independently through the tibia (shin) and femur (thigh) so the new graft can be placed.

*Tunnel placements illustrated are approximate locations
The New ACL
The new ACL is a graft called a bone-patellar tendon-bone graft. The middle 1/3 of the patellar tendon is removed with bone (bone plugs) from the knee cap (patella) and the shin (tibia) at both ends. We prefer to take the graft from the non-injured/opposite knee, called a contralateral graft. The graft can also be taken from the knee with the torn ACL, called an ipsilateral graft. If a contralateral graft is used, you will have a similar incision in the front of the knee.

Inserting The New ACL
Each of the bony ends are inserted into the tunnels and the graft is pulled into place. Sutures are attached to the bone plugs and then tied over buttons to hold the graft in place. A light dressing is applied and the patient is taken to a private room for an overnight stay. Before being dismissed from the hospital, the postoperative rehabilitation program is outlined and demonstrated for both the patient and family.

ACL Rehabilitation
POST-OP Physical Therapy
Time frames and exercises, as described below, are general guidelines and will be tailored to meet individual progress. The physical therapist/athletic trainer you work with before surgery is usually the same therapist that will follow you after surgery.
Day of Surgery
After surgery, your ACL-reconstructed knee will be placed in a continuous passive motion (CPM) machine, which gently moves your knee for you. The CPM machine is also used to elevate the knee above the heart to reduce swelling. A Cryo-cuff® will be placed on your knee, which is a cold compression device that helps to decrease pain and swelling after surgery.
You will start physical therapy the same day of surgery with a physical therapist in the hospital. Physical therapy will include range of motion exercises on the ACL knee and strengthening exercises on the donor-graft knee.
An advantage to taking the graft from the opposite knee is that the knee does not get swollen or lose motion after surgery; therefore, it allows the patient to start strengthening exercises immediately after surgery.
One Day POST-OP
Before leaving the hospital the day after surgery, the following conditions must be met:
- Full extension of the ACL-reconstructed leg equal to the donor-graft leg.
- Flexion of at least 120 degrees on the ACL-reconstructed leg and full flexion on the donor-graft leg.
- Ability to lift both legs independently.
- Ability to walk safely (with or without the use of crutches for balance).
- Understanding of home instructions for the next week.
Days 1-7 POST-OP
The first 7 days after surgery is considered to be a “bedrest” period, where we want you to stay in bed as much as possible in order to prevent swelling and allow you to work on the rehab exercises more effectively.
Rehab goals for this week include:
- Remain in bed with ACL-reconstructed leg elevated above heart in CPM machine.
- Maintain full extension of ACL-reconstructed leg.
- Maintain at least 120 degrees of flexion on ACL-reconstructed leg.
- Maintain full flexion on donor-graft leg.
- Ability to lift legs independently.
- Progression with Shuttle press on donor-graft leg to work on increasing strength.
Days 7-14 POST-OP
You will return to the office for your first post-op visit 1 week after surgery. At this time, your dressings will be changed. We will check your progress within the first week, instruct you on new rehab exercises, and educate you on how to gradually increase your activity level in the second week.
Most patients are able to gradually resume their normal daily activity during this week. How quickly you are able to resume normal activities is dependent on your ability to prevent swelling in your ACL-reconstructed knee and soreness in your donor-graft knee.
You will continue to perform rehab exercises three times a day. Exercises emphasize maintaining full extension and progressing with flexion on the ACL-reconstructed knee and progressing with strengthening on the donor-graft knee.
Two to Four Weeks POST-OP
During weeks 2-4, more emphasis is placed on strengthening the graft knee. Patients also continue working on ACL knee range of motion and keeping swelling down.
At 4 weeks, patients begin some form of low-impact conditioning exercise, such as riding a stationary bike, elliptical machine, etc. We will perform testing to check your stability and strength in order to provide patients with an individual program according to your needs and goals.
Two to Twelve Months POST-OP
Physical therapy will continue as the patient returns to their pre-operative level of activity. Strength, range of motion, and swelling will continue to be evaluated at each visit. Rehabilitation and sporting activities will be advanced as strength, comfort, and confidence allows.
Follow-up visits are typically every 2-3 months depending on your progress, but can occur more frequently if deemed necessary by your physical therapist/athletic trainer.
The following goals must be met prior to return to full, unrestricted activity:
- Full, symmetrical range of motion in the ACL-reconstructed compared to the donor-graft knee.
- No swelling in the ACL-reconstructed knee.
- Symmetrical strength with objective testing to within 10% side to side.
- Return of strength to within 10% of pre-op levels.
Helping Us Improve Care for Other Patients
Our current treatment of ACL injuries is based on our research. We’ve learned what works best by following patients after they finish their rehab.
We hope that you will be part of our research so we can help other patients in the future.
You can do this by taking our annual surveys and coming back for free follow-up visits at 2, 5, 10, 15, and 20 years after surgery.
