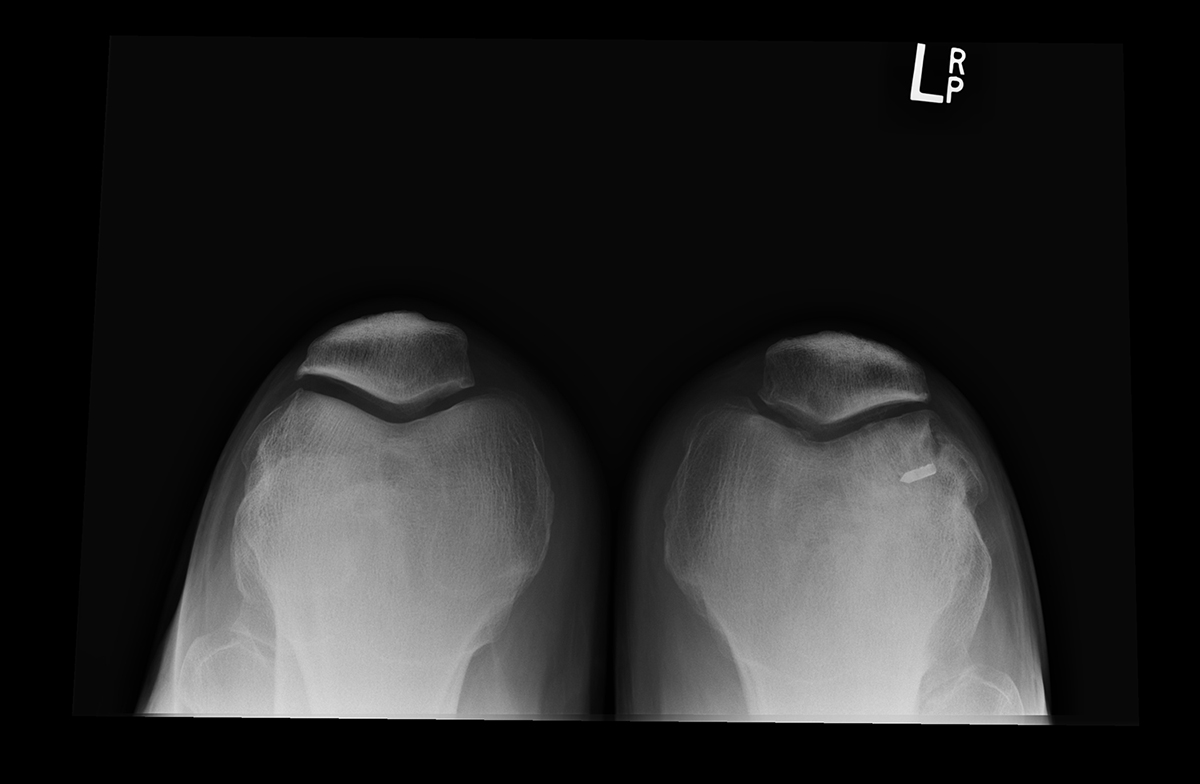
The benefit of treating just one thing is that you can become more familiar with a problem and the trends that occur. Although patellar dislocations are not common problems, we see a larger number of them because we only treat knee conditions and injuries. The average orthopedic surgeon may see fewer than 10 a year if that. But with 40 years of experience treating only knees, we’ve been able to develop a sound algorithm for treating patellar dislocations and/or malalignments that may be congenital in nature. Following a patellar dislocation, X-rays should include views of bilateral knees, especially the lateral and a merchant view (top image, above), not a sunrise view (bottom image, above), and lateral quad active view. We have been able to collect enough data to know what normal tendon lengths, patellae widths, normal alignment of patellae and trends between acute verses chronic dislocations. Surgeons who only see 2-3 patients with this diagnosis per year may overlook these anatomical findings and treat every dislocation the same.
A clear understanding of the anatomy and mechanics of the patellofemoral joint is critical when treating a patient who presents with a possible patellar dislocation. The alignment of the patellae should be evaluated to understand the relation of the patellae in the trochlea (the part of the femur that it sits in) medially and laterally, as well as looking at the height of the patellae, proximal to distal. Physical exam should include assessing for anatomical differences such as a “J” sign, the patella height and patella tilt and comparing to the opposite knee. The evaluation of both physical exam and radiographic exam should include the integrity of the medial retinaculum (a band of thickened deep fascia around tendons that holds them in place), the height of the patella, the length of the patellar tendon of the involved knee relative to the uninvolved knee. The treatment of patellar dislocations can depend on whether the problem is chronic or acute, and if the incident was traumatic or non-traumatic. If dislocations are occurring on one knee, comparing to the opposite knee can show what is different.
An MRI scan further evaluates the status of the medial retinaculum and seen on the axial view, and we can look for any chondral defects of the patellofemoral joint as well.
Treatment is dependent on the physical exam, X-ray measurements and MRI results. There are three options for patellar realignments:
- Medial Imbrication with Lateral Release(MI/LR)
- Usually done with acute dislocation and normal anatomy
- Soft issue correction only and no bony changes
- Release the lateral retinaculum and tighten medially to realign patella
- Patient wears an immobilizer when walking the first 1-2 weeks depending on quad control
- Bedrest with CPM with exercises of taking to 120 on CPM, SLR, 3x/day during the first week to minimize swelling and pain
- Elmslie Trillat Procedure (Trillat)
- Usually done with acute dislocation but patella sitting laterally but normal patellar tendon length
- Tibial tubercle is cut and moved medially (pivot)
- Fixed with plate and screws
- Will also do a MI/LR as above
- Bedrest with CPM with exercises of taking to 120 on CPM and SLR 3x/day.
- Distalization Procedure
- Usually done with acute/chronic dislocation with patella alta
- Tibial tubercle is cut and moved distally and medially (if indicated)
- Fixed with plate and screws
- Will also do the MI/LR as above
- Patient wears the immobilizer when walking the first 3-4 weeks
- Flexion limited to 90 degrees max (or lower based on tolerance) for CPM exercise 3x/day
- Will also do quad sets but no SLR as an exercise 3x/day. Assist lifting the leg in and out of CPM during first week of bedrest.
The purpose of bedrest in the first week with the use of CPM is more about controlling the effusion in the knee joint which allows us to be more aggressive starting week two (refer to our Blog on CPM use during first week). Our outcomes show the IKDC 2 years post op is 84 out of 100. By one week, patients have full symmetrical extension and by 4-6 weeks, they demonstrate symmetrical flexion. The mean strength at three months post op show 70% of 110 patients got greater than or equal to 90% of their pre-op strength, and 12% of those patients had strength between 80-89%.

